Major Surgeries Done: Primary Hip and Knee replacements (ceramic on ceramic, ceramic on X3 poly and metal on metal)
Follow Us

Innovative surgical and non-surgical treatments
to keep you in motion

Quality and Innovative Orthopaedic Care

Restoring Flexibility to your Spine
ARTHROSCOPY
REPLACEMENT
SURGERIES
SPINE
SHOULDER
FRACTURES
Arthroscopy
Arthroscopy is done through small incisions. During the procedure, your orthopaedic surgeon inserts the arthroscope (a small camera instrument about the size of a pencil) into your knee joint. The arthroscope sends the image to a television monitor. On the monitor, your surgeon can see the structures of the knee in great detail.
Your surgeon can use arthroscopy to feel, repair or remove damaged tissue. To do this, small surgical instruments are inserted through other incisions around your knee.

Knee Arthroscopy
Description
Arthroscopy is a common surgical procedure in which a joint(arthro-) is viewed (-scopy) using a small camera. Arthroscopy gives doctors a clear view of the inside of the knee. This helps them diagnose and treat knee problems.
Technical advances have led to high definition monitors and high resolution cameras. These and other improvements have made arthroscopy a very effective tool for treating knee problems. According to the American Orthopaedic Society for Sports Medicine, more than 4 million knee arthroscopies are performed worldwide each year.
Shoulder Arthroscopy
Shoulder arthroscopy is surgery that uses a tiny camera called an arthroscope to examine or repair the tissues inside or around your shoulder joint. The arthroscope is inserted through a small incision (cut) in your skin.

The rotator cuff is a group of muscles and tendons that cover your shoulder joint. These muscles and tendons hold your arm in your ball and socket shoulder joint, and they help you move your shoulder in different directions. The tendons in the rotator cuff can tear when they are overused or injured.
Most people receive general anesthesia before this surgery. This means you will be unconscious and unable to feel pain. Or, you may have regional anesthesia. Your arm and shoulder area will be numbed so that you do not feel any pain in this area. If you receive regional anesthesia, you will also be given medicine to make you very sleepy during the operation
First, your surgeon will examine your shoulder with the arthroscope. Your surgeon will:
Insert the arthroscope into your shoulder through a small incision. The arthroscope is connected to a video monitor in the operating room.
Inspect all the tissues of your shoulder joint and the area above the joint -- the cartilage, bones, tendons, and ligaments.
Repair any damaged tissues. To do this, your surgeon will make 1 - 3 more small incisions and insert other instruments through them. A tear in a muscle, tendon, or cartilage will be fixed. Damaged tissue may need to be removed.
Description
Replacement Surgeries
Total knee replacement is a surgery to restore the damaged segment of your knee and “IMPROVE QUALITY OF LIFE”. It makes you independent of managing your self, makes you less dependable , increases mobility and most importantly relives you of your pain and prolonged medication.
Once decided for knee replacement the most important thing is know what the surgery can do for you and its limitations which will be explained in detail during consultations. The complete pre operative ,post surgical and rehabilitation procedure will be explained in person and the things to expect and things you can perform and the don’ts’s will be explained. After knee replacement patientshav e a dramatic improvement in their pain and overall mobility and movement. The total nee replacement only allows good range of movments for your knee but will not be able to replicate what functions you had at knee before developing arthritis.
When Surgery is warranted ?
Surgical Procedure
Total knee replacement actually does not mean removing a big part of your knee and replacing with mwtal prosthesis. What actually is done is only a few milli meter of the damaged cartilage and bone is removed from your thigh bone[FEMUR] and Leg bone[Tibia]and Knee cap[PATELLA] and replaced with metal prosthesis. The most important step in total knee replacement is your soft tissue balancing which has to be prciscise for better function of your knee. That’s why total knee replacement is considered more of a soft tissue procedure than bony procedure.
The basic steps are:
> Removing of excessive new bones which restrict your knee movement and irritate your muscles and ligament
> Precision bone cuts
> Soft tissue balancing
> Checking stability of joints with trial prosthesis
> Wound wash and irrigation
> Cementing the new metal prosthesis
> Wound closure
Rehablitation
Patient is made to stand and walk according to their recovery on the same day or the next.
Muscle streghtening and stretches are started .
Special precations are taken for preventive measures of complications.
Complications
Immediate
> Infection
> Skin necrosis
> Wound Infection
Late
> Infection
> Aseptic lossening
> Implant wear
> Myositis
> Implant Breakage

> When pain and stiffness restricts your day to day activity and when conventional treatment like
medication, physiotherapy and intra articular supplements fail .
> When there is deformity of the knee associated with pain sometimes even at rest
> To avoid any chances of fracture due to mechanical instability at the kee.
Causes
The most disabling problem in the knee is arthritis. The different causes why arthritis happens in knee are
> Osteoarthritis
> Rheumatoid Arthritis
> Post traumatic arthritis
> Post septic sequel
> AVN

Total Hip Replacement Surgery
Hip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant. Hip replacement surgery can be performed as a total replacement or a hemi (half) replacement. Such joint replacement orthopaedic surgery is generally conducted to relieve arthritis pain or fix severe physical joint damage as part of hip fracture treatment. A total hip replacement (total hip arthroplasty) consists of replacing both the acetabulum and the femoral head while hemiarthroplasty generally only replaces the femoral head. Hip replacement is currently the most common orthopaedic operation, though patient satisfaction short and long term varies widely.
Total hip replacement is most commonly used to treat joint failure caused by osteoarthritis. Other indications include rheumatoid arthritis, avascular necrosis, traumatic arthritis,protrusio acetabuli, certain hip fractures, benign and malignant bone tumors, arthritis associated with Paget's disease, ankylosing spondylitis and juvenile rheumatoid arthritis. The aims of the procedure are pain relief and improvement in hip function. Hip replacement is usually considered only after other therapies, such as physical therapy and pain medications, have failed.


Bipolar Hip Hemi replacements
Treatment for femoral neck fractures can be successfully achieved through a bipolar hemiarthroplasty. Hemiarthroplasty is a surgical procedure that replaces one half of the hip joint with a prosthetic, while leaving the other half intact. There are several different options available for the type of device to be used; we prefer to use a bipolar type, which has a femoral head that swivels during movement. This helps to reduce the amount of wear and tear on the new joint for longer lasting results however with limited indications.
During the hemiarthroplasty procedure, the damaged femoral head and neck are removed and replaced with the bipolar prosthetic. The prosthetic may be held in place with or without cement. Patients will need to undergo physical therapy after surgery to help restore movement and function to the joint. Therapy begins as soon as the patient feels comfortable after surgery, which is often the very next day. Most patients experience effective, long-term results from this procedure.
Hip Bipolar Hemiarthroplasty for Femoral Neck Fracture
Fractures of the hip often occur within the femoral neck, a thin section of the thigh bone that helps to connect the “ball” end of the bone to the main shaft. When a fracture occurs in this area of the bone, it can cut off blood supply that cannot be treated with conservative methods.

Revision Hip and Knee replacements
Over the past 3 decades there has been an increases trend in Hip and knee replacements. Millions of people around the world has undergone hip an knee replacement for various ailment. These prosthesis tend to wear out or fail due to various reasons in a very small amount of population. When these prosthesis are removed and replaced with new and more stable implants this procedure is known as revision replacement surgery.
Indication
> Wear
> Aseptic loosening
> Infection
> Trauma or fracture
> Improper technique during primary surgery
> Implant breakage
Surgery
Revision surgery is complex and requires good skills and knowledge about the reconstruction of the joint.
The basics steps are to do careful and a clean dissection, assessing the bone stalk, implant removal, bone loss assessment, removing fibrous tissue, soft tissue balancing, fitting trial implants and checking stability, joint lavage, fitting new implant and wound closure
Complications
> Infection
> Stiffness
> Dislocations
> DVT
Spine
Anterior cervical corpectomy and discectomy / fusion

Anterior cervical discectomy and fusion (ACDF) is a surgical procedure to treat nerve root or spinal cord compression by decompressing the spinal cord and nerve roots of the cervical spine in order to stabilize the corresponding vertebrae. This procedure is used when other non-surgical treatments have failed.
The nucleus pulposus (the jelly-like center of the disc) of the herniateddisc bulges out through the annulus (surrounding wall) and presses on the nerve root next to it. This nerve root becomes inflamed and causes serious pain. The problem can also be caused by degenerative disc disease (spondylosis). The disc consists of about 80% water. When one grows older, the disc starts to dry out and shrink, causing small tears in the annulus and inflammation of the nerve root.

What is Anterior Cervical Corpectomy Fusion?
Anterior Cervical Corpectomy Fusion is a surgery to fix he bones in your neck together to steady it or prevent movement. The surgeon makes an incision in the front of your neck to remove all or some of the vertebrae, place a cage, or graft in the disc space, and then place a titanium plate across that space to hold it. The pressure on the spinal cord and/or nerves is relieved by taking out any disc or bony material that might be pushing on them before the neck is fused together.
Most patients stay in the hospital for 2-3 days. Before you can go home, you need to be able to:
1. Control your pain by taking oral pain medications
2. Get up and walk around on your own
3. Empty your bladder.
If you are unable to do these activities or if you have any problems from your surgery, you may need to stay in the hospital longer.
The neurosurgeon or orthopedic surgeon enters the space between two discs through a small incision in front (= anterior) of and at the right or left side of the neck. The disc is completely removed, as well as arthriticbone spurs. The disc material, pressing on the spinal nerve or spinal cord, is then completely removed. The intervertebral foramen, the bone channel through which the spinal nerve runs, is then enlarged with a drill giving the nerve more room to exit the spinal canal.
To prevent the vertebrae from collapsing and to increase stability, the open space is often filled with bone graft, The slow process of the bone graft joining the vertebrae together is called "fusion". Sometimes a titanium plate is screwed on the vertebrae or screws are used between the vertebrae to increase stability during fusion, especially when there is more than one disc involved.
The surgery requires a short stay in the clinic (1 to 3 days) and a gradual recovery between 1 to 2 weeks. The patient may be advised to wear a neck brace or collar (for up to 8 weeks) that serves to ensure proper spinal alignment. Wearing the brace heightens one's awareness of posture and positioning and helps prevent movements (e.g., sudden and/or excessive bending or twisting of the neck) that may aggravate or slow down the healing process. It is especially advisable to wear a protective neck brace when traveling (e.g., by car), sleeping, showering, or any other activities in which the patient may not be able to be ensure proper spinal alignment. In addition, physical therapy and related healing modalities (e.g., massage, acupuncture) may be recommended in order to promote proper healing, as well as to strengthen the surrounding muscles that can take over the neck brace's 'job' of ensuring proper spinal alignment when the patient starts (around 4 to 6 weeks after surgery) to wean off the neck brace.
Cervical disc replacement surgeries
Your cervical spine is made up of the seven bones, called cervical vertebrae, stacked on top of each other in your neck area. The cervical disks are the cushions that lie between the cervical vertebrae and act as shock absorbers to allow your neck to move freely.
Your cervical spine also forms a protective tunnel for the upper part of your spinal cord to pass through. As your spinal cord passes through this tunnel, it sends out spinal nerves that pass through the openings between the cervical vertebrae. These spinal nerves supply your upper body with sensation and movement.
Cervical disk replacement surgery involves removing a diseased cervical disk and replacing it with an artificial disk. It is done when the part of your vertebrae or your cervical disk is pressing on your spinal cord or spinal nerves, causing you pain, numbness, or weakness. When these symptoms do not respond to nonsurgical types of treatment, disk surgery may be recommended.
Using an artificial disk to replace your natural cervical disk is a new type of treatment that has recently been approved by the FDA. In traditional cervical disk surgery, the diseased disk is removed and the cervical vertebrae above and below the disk may be fused together. Disk replacement surgery may have the advantage of allowing more movement and creating less stress on your remaining vertebrae than traditional cervical disk surgery.
Reasons for the procedure
Cervical disk degeneration, or wear and tear, is common. Cervical disks begin to collapse and bulge with age; this happens to most people by age 60. But doctors don’t know why some people have more symptoms from cervical disk degeneration than others.
Your symptoms may include:
> Neck pain
> Neck stiffness
> Pain that travels down into your shoulders or into your arms
> Weakness of your shoulders, arms, hands, or legs
> "Pins and needles" or numbness in your arms
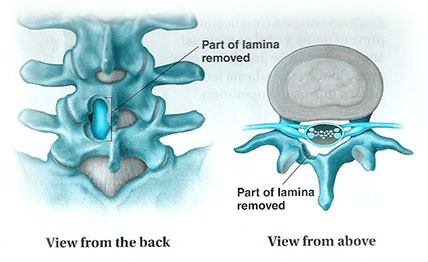
Micro Discectomies
Microdiscectomy

Discectomy
A discectomy (also called open discectomy) is the surgical removal of herniated disc material that presses on a nerve root or the spinal cord. The procedure involves removing the central portion of an intervertebral disc, the nucleus pulposus, which causes pain by stressing the spinal cord or radiating nerves.
The traditional open discectomy, or Love's technique, was published by Ross and Love in 1971. Advances in options have produced effective alternatives to traditional discectomy procedures (i.e. Microdiscectomy, Endoscopic Discectomy, and Laser Discectomy). In conjunction with the traditional discectomy, a laminotomy is often involved to permit access to the intervertebral disc. In this procedure, a small piece of bone (the lamina) is removed from the affected vertebra, allowing the surgeon to better see and access the area of disc herniation.
Microdiscectomy is a minimally invasive surgical procedure in which a portion of a herniated nucleus pulpolsus is removed by way of a surgical instrument or laser while using an operating microscope or loupe for magnification.
Anterior lumbar interbody fusion (ALIF) is a type of spinal fusion that utilizes an anterior (front - through the abdominal region) approach to fuse (mend) the lumbar spine bones together. Interbody fusion means the intervertebral disc is removed and replaced with a bone (or metal) spacer, in this case using an anterior approach.
The anterior technique is often favored when multiple spinal levels are being fused and multiple discs need to be removed. ALIF may be performed in conjunction with or without a posterior decompression (laminectomy) and/or instrumentation (use of metal screws/rods).
The anterior ALIF approach is also ideal when only one spinal level is fused and a posterior decompression and/or instrumentation are not required. Although the anterior lumbar ALIF approach involves retracting (moving out of the way, temporarily) large blood vessels (aorta, vena cava) and the intestines, there is a wide exposure of the intervertebral disc without retraction of the spinal nerves and neurologic structures (and therefore, a decreased risk of neurologic injury).
The surgery is performed utilizing general anesthesia. A breathing tube (endotracheal tube) is placed and the patient breathes with the assistance of a ventilator during the surgery. Preoperative intravenous antibiotics are given. Patients are positioned in the supine (lying on the back) position, generally using a special, radiolucent operating table. The surgical region (abdominal area) is cleansed with a special cleaning solution. Sterile drapes are placed, and the surgical team wears sterile surgical attire such as gowns and gloves to maintain a bacteria-free environment.
The intervertebral disc is then removed using special biting and grasping instruments (such as a pituitary rongeur, kerrison rongeur, and curettes). Special distractor instruments are used to restore the normal height of the disc, as well as to determine the appropriate size spacer to be placed. A bone spacer (metal or plastic spacers may also be used) is then carefully placed in the disc space. Fluoroscopic x-rays are taken to confirm that the spacer is in the correct position.
The wound area is usually washed out with sterile water containing antibiotics. The deep fascial layer and subcutaneous layers are closed with a few strong sutures. The skin can usually be closed using special surgical glue, leaving a minimal scar and requiring no bandage.
The total surgery time is approximately 2 to 3 hours, depending on the number of spinal levels involved.
Overview and Indications
Surgical Technique

Posterior lumbar interbody fusion surgeries.
Spinal fusion is a surgical procedure used to correct problems with the small bones in the spine (vertebrae). It is essentially a "welding" process. The basic idea is to fuse together the painful vertebrae so that they heal into a single, solid bone.
As with all spinal fusion surgery, a posterior lumbar interbody fusion (PLIF) involves adding bone graft to an area of the spine to set up a biological response that causes the bone to grow between the two vertebral elements and thereby stop the motion at that segment.
Unlike the posterolateral gutter fusion, the PLIF achieves spinal fusion in the low back by inserting a cage made of either allograft bone or synthetic material (PEEK or titanium) directly into the disc space. When the surgical approach for this type of procedure is from the back it is called a posterior lumbar interbody fusion (PLIF).
A PLIF fusion is often supplemented by a simultaneous posterolateral spine fusion surgery.
Description
First, the spine is approached through a three-inch to six-inch long incision in the midline of the back and the left and right lower back muscles (erector spinae) are stripped off the lamina on both sides and at multiple levels.
After the spine is approached, the lamina is removed (laminectomy) which allows visualization of the nerve roots. The facet joints, which are directly over the nerve roots may then be undercut (trimmed) to give the nerve roots more room.
The nerve roots are then retracted to one side and the disc space is cleaned of the disc material.
A cage made of allograft bone, or posterior lumbar interbody cages with bone graft, is then inserted into the disc space and the bone grows from vertebral body to vertebral body.
PLIF Potential Advantages and Disadvantages

Doing a pure PLIF surgery has the advantage that it can provide anterior fusion of the disc space without having a second incision as would be necessary with an anterior/posterior spine fusion surgery. However, it has some disadvantages:
Not as much of the disc space can be removed with a posterior approach (from the back).
An anterior approach (an ALIF, from the front) provides for a much more comprehensive evacuation of the disc space and this leads to increase surface area available for a fusion.
A larger spinal implant can be inserted from an anterior approach, which provides for superior stabilization.
In cases of spinal deformity (e.g. isthmic spondylolisthesis) a posterior approach alone is more difficult to reduce the deformity.
There is a small but finite risk that inserting a cage posteriorly will allow it to retro pulse back into the canal and create neural compression.
PLIF surgery has a higher potential for a solid fusion rates than posterolateral fusion rates because the bone is inserted into the anterior portion (front) of the spine. Bone in the anterior portion fuses better because there is more surface area than in the posterolateral gutter, and also because the bone is under compression. Bone in compression heals better because bone responds to stress (Wolff's law), whereas bone under tension (posterolateral fusions) does not see as much stress.

Transforaminal lumbar interbody fusions with instrumentation.

Spinal fusion (such as a TLIF) is a surgical technique to stabilize the spinal vertebra and the disc or shock absorber between the vertebra. Lumbar fusion surgery is designed to create solid bone between the adjoining vertebra, eliminating any movement between the bones. The goal of the surgery is to reduce pain and nerve irritation.
Reasons for TLIF Surgery:
> Spondylolisthesis
> Degen. Disc Disease
> Herniated Disc
Spinal fusion may be recommended for conditions such as spondylolisthesis,
degenerative disc disease or recurrent disc herniations. Surgeons
perform lumbar fusion using several techniques.
Benefits of TLIF Back Surgery Technique
> TLIF procedure has several theoretical advantages over some other forms of lumbar fusion:
> Bone fusion is enhanced because bone graft is placed both along the gutters of the spine posteriorly but also in the disc space.
> A spacer is inserted into the disc space helping to restore normal height and opening up nerve foramina to take pressure off the nerve roots.
> A TLIF procedure allows the surgeon to insert bone graft and spacer into the disc space from a unilateral approach laterally without having to forcefully retract the nerve roots as much, which may reduce injury and scarring around the nerve roots when compared to a PLIF procedure.
As with all forms of lumbar spine fusion, prior to TLIF surgery medical clearance is obtained. Smoking should be stopped. Patients may require pre-donation of blood to be used at the time of surgery.

Shoulder Arthroplasty
Total shoulder replacement is indicated for two main diagnostic groups:
> Rheumatoid arthritis
> Osteoarthritis (primary and secondary)

Description
Among the causes of secondary osteoarthritis are the effects of old trauma, postdisloca-tion arthropathy, cuff tear arthropathy, congenital dysplasia, the effects of old sepsis, and osteonecrosis. More rarely, surgery is indicated for tumor and failed surgery (including revision of previous prosthesis). Whatever the cause of the destructive process on the articular surface, the net result remains the same, that is increasing pain and stiffness. The overwhelming indication for surgery is uncontrolled pain 'with loss of movement and consequent loss of function. The expectations for shoulder replacement are higher than for lower limb joint replacements. If in the hip and knee, for instance, a stable pain-free joint with two-thirds range of motion is achieved, then this is seen as an excellent result. At the shoulder, however, being stable and pain free is not enough. It is the most mobile joint in the body, and hence a much greater range of mobility is expected.
The results of shoulder replacement depend almost entirely on the adequacy of soft tissues and musculature and restoration of the anatomic geometry of the joint. This cannot be so easily achieved at the shoulder as it can at either hip or knee. When assessing a shoulder before replacement, it is often thought that there is a complete loss of rotator cuff. There may indeed be loss of rotator cuff function, but this does not imply discontinuity. Often, because of gross erosion of joint surfaces, the center of rotation has been medialized and hence the rotator cuff defunction. If the rotator cuff has lost its action, then the unopposed deltoid has its resolution of forces directed superiorly, and hence upward subluxation of the humoral head results. If this process can be reversed, that is, by lateralization of the center of rotation by retensioning both cuff and deltoid, then restoration of function can be expected. Unfortunately, in the most severely affected joints, long-term adaptive changes have occurred, that is, shortening of rotator cuff muscles; therefore, complete restoration of geometry by lateralization of the center of rotation is not possible, because the soft tissues cannot be elongated adequately to the anatomic position.
In the more severe cases, loss of the rotator cuff may indeed be true and complete. In this situation, it may be wiser to consider hemiarthroplasty alone because the incidence of glenoid loosening in the face of complete rotator cuff loss is greater. This can be surmised on a mechanical basis alone. If the rotator cuff is not present, the humeral head is subluxed superiorly. If the glenoid replacement is then placed in the anatomic position, a rocking or toggle movement increases the chance of loosening. Interestingly, the results of hemiarthroplasty in relation to total replacement are not too dissimilar. However, it has been shown that hemiarthroplasty alone may not give the complete relief of pain experienced by the total replacement.
All shoulder replacements of whatever design require good bone stock for fixation of the glenoid component. If medial erosion of the glenoid has occurred such that the erosion is to the base of the coracoid, then it is unlikely that adequate seating of the glenoid component ¦will be achieved, and it may be better in this situation to accept the hemiarthroplasty alone.
Shoulder
Fractures
Dynamic hip screw fixation
Dynamic hip screw (DHS) or Sliding Screw Fixation is a type of orthopaedicimplant designed for fixation of certain types of hip fractures. which allows controlled dynamic sliding of the femoral head component along the construct. The idea behind the dynamic compression is that the femoral head component is allowed to move along one plane; since bone responds to dynamic stresses, the native femur may undergo remodeling and proper fracture healing.
Assembled dynamic hip screw. The lag screw for the femoral head is within in sleeve of the side plate. The side plate shows the fixation screws that are inserted into the femoral diaphysis. The two upper screws are cancellous screws and lower four screws are cortical screws.
Dynamic hip screw transfixing an intertrochanteric fracture of the right femur. A cannulated cancellous screw that serves as a lag screw has also been inserted to increase compression and to control rotation of the femoral head. Note the lesser trochanter has been fractured off the femur and has been displaced medially.
Dynamic hip screws are used for internal fixation of fractures of the femoral neck and intertrochanteric region. The screw is a large cancellous lag screw that glide freely in a metal sleeve. The sleeve is attached to a side plate that is fixed to the lateral femoral cortex with screws. Weight bearing cause the femoral head to becomes impacted on the femoral neck producing dynamic compression of the fracture. The shaft of the lag screw slides down the sleeve maintaining reduction of the fracture as compression occurs.

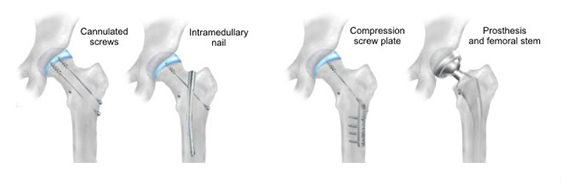
A hip fracture is a break in the upper quarter of the femur (thigh) bone. The extent of the break depends on the forces that are involved. The type of surgery used to treat a hip fracture is primarily based on the bones and soft tissues affected or on the level of the fracture.
Internal fixation is an operation in orthopedics that involves the surgical implementation of implants for the purpose of repairing a bone, a concept that dates to the mid-19th century and was made applicable for routine treatment in the mid-20th century. An internal fixator may be made of stainless steel or titanium.
Types of internal fixators include bone screws and metal plates, pins, rods,[3] Kirschner wires and intramedullary devices such as the Kuntscher nail and interlocking
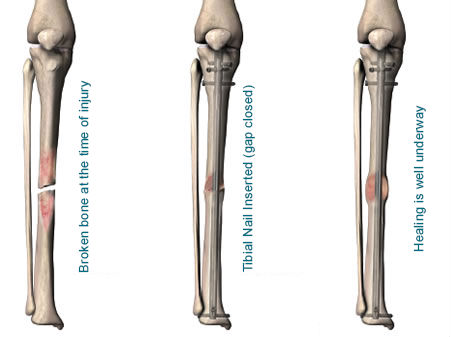
Open Reduction Internal Fixation (ORIF) involves the implementation of implants to guide the healing process of a bone, as well as the open reduction, or setting, of the bone itself. Open reduction refers to open surgery to set bones, as is necessary for some fractures. Internal fixation refers to fixation of screws and/or plates, intramedullary bone nails (femur, tibia, humerus) to enable or facilitate healing. Rigid fixation prevents micro-motion across lines of fracture to enable healing and prevent infection, which happens when implants such as plates (e.g. dynamic compression plate) are used. Open Reduction Internal Fixation techniques are often used in cases involving serious fractures such as comminuted or displaced fractures or in cases where the bone would otherwise not heal correctly with casting or splinting alone.
Risks and complications can include bacterial colonization of the bone, infection, stiffness and loss of range of motion, non-union, mal-union, damage to the muscles, nerve damage and palsy, arthritis, tendonitis, chronic pain associated with plates, screws, and pins, compartment syndrome, deformity, audible popping and snapping, and possible future surgeries to remove the hardware.
Open reductions of Intraarticular fracture fixations/external fixation application


The most significant advances in treatment during the 20th century is the development of internal fixation which ranked high on the list.
Internal fixation allows shorter hospital stays, enables individuals to return to function earlier and reduces the incidence of nonunion (improper healing) and malunion (healing in improper position).
A broken bone must be carefully fixed in position and supported until it is strong enough to bear weight. Until the last century, physicians relied on casts and splints to support the bone from outside the body (external fixation). But the development of sterile surgery reduced the risk of infection so that doctors could work directly with the bone and could implant materials in the body.
New materials such as stainless steel, cobalt and titanium were not only durable, but also had the strength and the flexibility necessary to support the bone. These materials are also compatible with the body and rarely cause an allergic reaction or implant failure.
The most common types of internal fixation are wires, plates, rods, pins, nails, and screws used inside the body to support the bone directly.
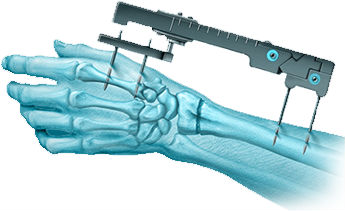
Internal Fixation for Fractures
External Fixation for Fractures